Information on Maintaining Eligibility
In October 2017, the North Carolina Department of Health and Human Services (DHHS) implemented a quarterly Maintain Eligibility Process through NCTracks. This process identifies enrolled providers with no claim activity within the past 12 months. NCTracks notifies the provider by a Notification of Inactivity Letter posted to the secure provider portal mailbox.
When a provider is identified as having no claims activity in 12 months, a Maintain Eligibility Due Date will be set. Providers will be notified 30 days before the due date that they must submit a Maintain Eligibility Application via a Notification of Inactivity Letter. Providers will not receive reminders about Maintaining Eligibility past the initial notification letter.
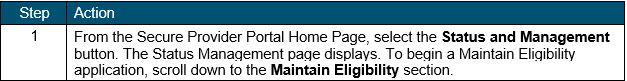
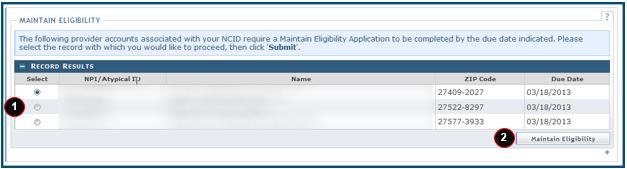
The Notification of Inactivity Letter provides guidance for completing the Maintain Eligibility Application on the secure NCTracks provider portal. Providers can see the application on the Status and Management Page in the Maintain Eligibility section located in the Secure Provider Portal. Upon submission of the Maintain Eligibility Application, the provider’s enrollment record will be updated with the current date.
If the provider does not submit the application by the due date, the provider’s participation in the North Carolina Medicaid and NC Health Choice programs will be end dated and a Provider Termination Letter will be sent by certified mail. The Maintain Eligibility Process will help prevent fraud, waste and abuse in the Medicaid and NC Health Choice programs.
The Maintain Eligibility Process reviews NCTracks history to see if the provider has been included on any claims over the last 12 months.
- Attending
- Billing
- Ordering
- Operating
- Other operating
- Prescribing
- Rendering
- Referring
- Service facility
*Keep in mind that providers who have a Manage Change Request (MCR) in review or a re-verification application submitted within the past year will not receive a letter for that quarter.
*Rural Health Clinics and Federally Qualified Health Centers are excluded from this requirement.
 NCTracks
NCTracks